What is an autorefractor test?
An autorefractor test is a type of eye examination used to determine the refractive status of the eye (eye’s refractive status) and provide a precise prescription for glasses or contact lenses. This technology has become an essential tool for optometrists, ophthalmologists, and other eye care professionals over the past few decades as it provides a much more accurate means of assessing a person’s vision than manual testing methods.
Autorefractors are digital instruments that measure refractive errors by utilizing highly advanced optical technology. The device works by sending light pulses into the patient’s eyes and then recording how the light is focused on their retina. It then determines any astigmatism, myopia, hyperopia, or presbyopia present in the eye and sends this information to the practitioner who can make an accurate assessment regarding vision correction.
The accuracy of autorefractors has been well documented over the years, with some studies suggesting they can even be more reliable than human refraction tests done by qualified practitioners. In one study conducted in 2015, autorefractors were able to determine refractive errors within 0.2 diopters of the accepted standard and even exceeded human error standards in certain cases. This makes these devices much more reliable than other technologies used to test refractive errors such as corneal topography or retinoscopy.
In addition to providing accurate results for glasses and contact lenses prescriptions, autorefractor tests offer many other important benefits as well. These devices are very effective at detecting subtle changes in a person’s vision over time which can alert doctors if there have been any significant changes since their last visit. This helps ensure that patients receive timely treatment when needed while avoiding unnecessary treatments or costs associated with inefficient care delivery processes.
Overall, autorefractor tests provide tremendous benefits for both patients and healthcare providers alike due to their accuracy and ability to detect subtle changes in a patient’s eyesight quickly and effectively. By combining data from multiple tests together, practitioners can gain valuable insights into their patient’s vision which helps optimize care delivery for better outcomes at lower costs.










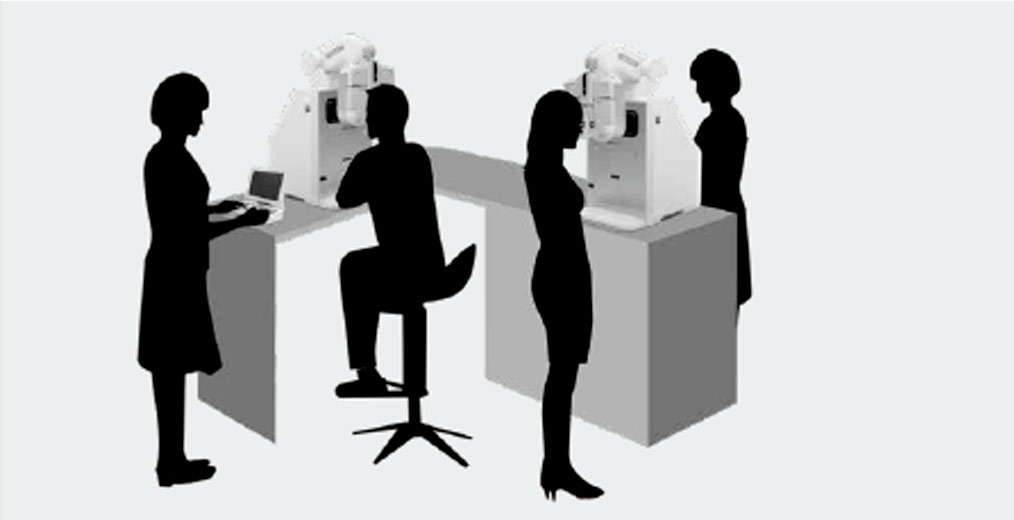 What about saving space? In times of taking care of our health, distance is very important for us, that’s why the TCP-1 is the most space-saving refraction unit for convenient use that comes with a infrared, WIFI and bluetooth remote control that will help you with a more avant-garde experience. But the best part of it is its compact appearance and sophisticated design due to its phoropter that lifts up and down automatically, improving by this your professional eye testing feeling and value.
What about saving space? In times of taking care of our health, distance is very important for us, that’s why the TCP-1 is the most space-saving refraction unit for convenient use that comes with a infrared, WIFI and bluetooth remote control that will help you with a more avant-garde experience. But the best part of it is its compact appearance and sophisticated design due to its phoropter that lifts up and down automatically, improving by this your professional eye testing feeling and value.
